Innovative solutions are reshaping the way we approach healthcare and emergency response. From predictive analytics to AI-driven diagnostics, these advancements are making a significant difference.
For instance, Kaiser Permanente’s predictive analytics have prevented over 520 deaths annually. Similarly, Mexico’s 911 system handles more than 3.5 million emergency calls every quarter, showcasing the efficiency of geolocation-enabled systems.
Localized medical device production in Africa is another example of how innovation is improving accessibility. These real-world cases highlight the measurable impact of technological advancements on mortality rates and system efficiency.
As we delve deeper, we’ll explore more examples from Kaiser Permanente, Mexico’s 911 system, and African medical device manufacturers. These stories underscore the transformative power of technology in saving lives.
Introduction: The Role of Technology in Saving Lives
The integration of cutting-edge systems is reshaping medical practices. These advancements are not replacing physicians but augmenting their capabilities. The American Medical Association (AMA) emphasizes that artificial intelligence serves as a tool to enhance, not replace, human expertise in healthcare.
Dr. Bruce Scott, a leading voice in medical innovation, highlights the importance of balancing progress with patient privacy.
“Innovation must align with ethical standards to ensure trust in healthcare systems,”
he states. This balance is critical as systems evolve to meet growing demands.
The World Health Organization (WHO) has issued an urgent call for localized medical device production. This initiative aims to address Sustainable Development Goals (SDGs) by improving access to essential tools in underserved regions. Challenges like the 81% diagnostic gap in low-income countries underscore the need for equitable solutions.
Physician burnout, often caused by data overload, is another pressing issue. Streamlining care through optimized systems can alleviate this burden. The discussion revolves around three key pillars:
- Clinical care optimization
- Emergency response acceleration
- Equitable medical access
These pillars form the foundation for leveraging technology to improve outcomes and save time in critical situations. As we explore these areas, the transformative potential of innovation becomes clear.
How Can Technology Save Lives in Healthcare?
Modern advancements are transforming patient care in hospitals. Digital tools and AI are now integral to improving outcomes and reducing risks. These innovations empower doctors to make faster, more accurate decisions.
Kaiser Permanente’s Advance Alert Monitor is a prime example. This system analyzes over 100 electronic health record (EHR) data points hourly. It has prevented an estimated 520 deaths annually by flagging at-risk patients 6-12 hours before clinical deterioration.
Predictive analytics are reshaping traditional care models. Instead of reactive treatments, doctors can now focus on preventive measures. This shift not only improves patient outcomes but also enhances the overall quality of care.
Digital Health Tools and AI in Patient Care
AI-powered systems are reducing the burden on doctors. For instance, Kaiser’s AI message routing has cut physician inbox burdens by 45%. This allows doctors to focus on critical cases, improving efficiency in hospitals.
The American Medical Association (AMA) is leading efforts to ensure AI reduces racial and gender bias in treatment recommendations. Their blueprint emphasizes equity and clinical environment improvements, ensuring fair access to care for all patients.
Predictive Analytics and Early Intervention
Predictive models are revolutionizing early intervention strategies. By analyzing patient data, these systems identify risks before they escalate. This proactive approach has led to significant improvements in diagnostic accuracy.
Telehealth integration with emergency routing is another breakthrough. It ensures time-sensitive cases receive immediate attention, saving valuable time in critical situations.
| Aspect | Traditional Care | AI-Enabled Care |
|---|---|---|
| Patient Monitoring | Manual, periodic checks | Continuous, real-time data analysis |
| Risk Identification | Reactive, after symptoms appear | Proactive, 6-12 hours before deterioration |
| Treatment Bias | Potential for human bias | AI reduces racial and gender bias |
Despite these advancements, cybersecurity remains a challenge. Protecting sensitive patient data is crucial to maintaining trust in healthcare systems. Hospitals must invest in robust security measures to safeguard information.
Enhancing Emergency Response with Technology
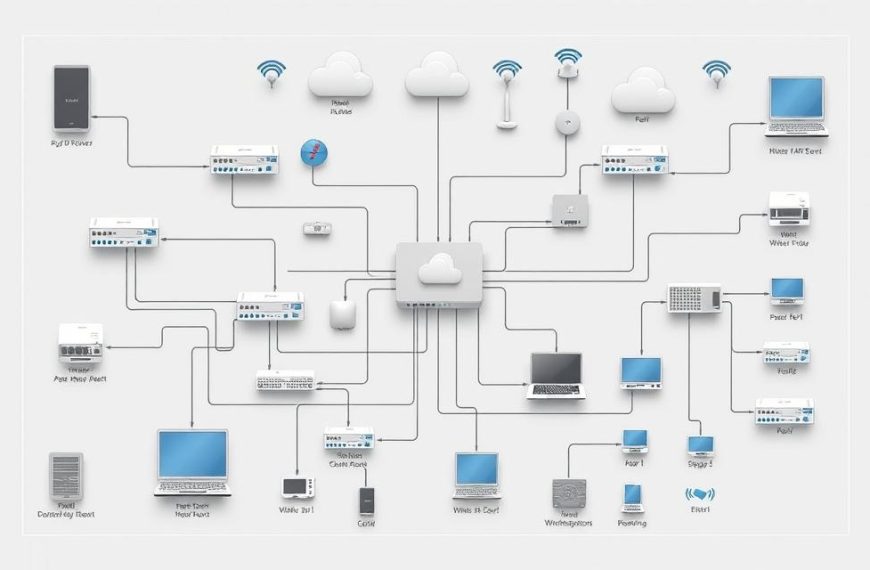
Emergencies demand swift and precise responses, and modern systems are rising to the challenge. From AI-powered call analysis to geolocation technologies, these advancements are transforming how emergencies are managed. Mexico’s centralized 911 system is a prime example of this evolution.
Previously, Mexico’s emergency response was hindered by multi-number confusion. Today, the system integrates AI to classify emergencies within the first 20 seconds of a call. This ensures the right assistance is dispatched quickly, saving valuable time.
AI-Powered Emergency Call Systems
Motorola’s VESTA 9-1-1 software is a game-changer. It uses AI to analyze calls, reducing response time significantly. The system also integrates voice recognition to categorize emergencies, ensuring accurate information is relayed to responders.
Training protocols blend AI analysis with human operator emotional intelligence. This combination ensures that both technical and emotional aspects of emergencies are addressed effectively.
Geolocation and Rapid Deployment
Geolocation technologies have improved location accuracy by 89% in scenarios like kidnappings or accidents. By triangulating cellular and WiFi signals, responders can pinpoint incidents with precision.
Motorola’s crisis response software enables multi-agency coordination. This ensures a unified approach to emergencies, enhancing overall efficiency.
| Aspect | Traditional Systems | AI-Enhanced Systems |
|---|---|---|
| Call Analysis | Manual, time-consuming | AI-driven, completed in 20 seconds |
| Location Accuracy | Limited by manual inputs | 89% improvement with geolocation |
| Response Coordination | Fragmented across agencies | Unified through multi-agency software |
Despite these advancements, challenges remain. Maintaining system uptime during peak call volumes, like Mexico’s 3.5 million calls per quarter, is critical. Continuous investment in technologies and training is essential to meet this need.
Improving Access to Medical Devices Worldwide
Access to essential medical devices remains a global challenge, especially in underserved regions. While 95% of high-income populations have access to basic diagnostics, only 19% in low and middle-income countries (LMICs) do. This disparity highlights the urgent need for equitable solutions.
Diagnostic gaps contribute to 1.1 million preventable deaths annually in LMICs. Addressing this issue requires tackling supply chain vulnerabilities and regulatory hurdles. For instance, 72% of African countries rely on imported devices, making them susceptible to disruptions.
Challenges in Medical Device Accessibility
Several barriers hinder access to medical devices in LMICs. Supply chain inefficiencies often delay the delivery of critical tools. Additionally, 68% of African nations lack frameworks for approving medical devices, creating regulatory bottlenecks.
High costs further exacerbate the problem. Imported devices are often unaffordable for local healthcare systems. Limited resources and trained staff also pose significant challenges, making it difficult to operate and maintain advanced equipment.
Localizing Production and Solutions
Localized production is emerging as a viable solution. For example, Revital Healthcare in Kenya produces 45 medical devices, including PPE and syringes, employing over 650 workers. This not only reduces costs but also strengthens local economies.
Ethiopia’s ultrasound assembly plant is another success story. By manufacturing locally, the country has reduced device costs by 40%. These initiatives demonstrate the potential of regional production hubs to improve accessibility.
Hybrid models combining local assembly with foreign partnerships can further enhance sustainability. For more insights, explore the World Bank’s strategies on medical device accessibility.
Conclusion: The Future of Life-Saving Technology
The future of healthcare and emergency response lies in the seamless integration of advanced systems. AI’s expansion into predictive public health monitoring offers immense potential for pandemic prevention. Investing $2.1 billion annually in LMIC medical device infrastructure, as proposed by the WHO, is crucial for bridging accessibility gaps.
Physician-AI collaboration models must preserve human judgment in critical care. Standardized emergency response protocols, integrating 5G and edge computing, will enhance efficiency. Global certification programs for climate-resilient medical equipment ensure sustainability in challenging environments.
Ethical considerations remain paramount. Advanced technologies must bridge, not widen, health equity gaps. By focusing on equitable solutions, we can harness the full potential of intelligence-driven systems to shape a safer, healthier future.
FAQ
What role does artificial intelligence play in healthcare?
Artificial intelligence enhances patient care by analyzing data, predicting risks, and assisting doctors in making informed decisions. It improves treatment outcomes and reduces costs.
How do digital health tools improve patient outcomes?
Digital health tools provide real-time information, streamline workflows, and support staff in delivering quality care. They help monitor patients and ensure timely interventions.
What are the benefits of predictive analytics in healthcare?
Predictive analytics identifies potential health risks early, allowing for proactive treatment. This reduces emergency cases and improves overall patient health.
How does technology enhance emergency response systems?
AI-powered emergency call systems and geolocation tools enable rapid deployment of resources. This ensures faster assistance during critical situations.
What challenges exist in accessing medical devices globally?
High costs, limited resources, and logistical issues hinder accessibility. Localizing production and innovative solutions can address these challenges.
How can medical device accessibility be improved worldwide?
By localizing production, reducing costs, and leveraging software solutions, medical devices can become more accessible to people in need.
What is the potential of AI in emergency call systems?
AI can analyze emergency calls, prioritize cases, and dispatch assistance efficiently. This saves time and improves response rates during crises.
How does geolocation technology aid in emergency situations?
Geolocation pinpoints the exact location of patients, enabling rapid deployment of emergency services. This is crucial for saving lives in critical moments.
What are the key applications of technology in healthcare?
Applications include AI diagnostics, remote monitoring, and data-driven treatment plans. These tools enhance care quality and reduce risks for patients.
How does technology address healthcare resource limitations?
By optimizing workflows, reducing costs, and improving efficiency, technology ensures better use of available resources in hospitals and clinics.